What Is Orthorexia? Causes, Warning Signs & Treatments

Throughout 2021, Good Housekeeping will be exploring how we think about weight, the way we eat, and how we try to control or change our bodies in our quest to be happier and healthier. While GH also publishes weight loss content and endeavors to do so in a responsible, science-backed way, we think it’s important to present a broad perspective that allows for a fuller understanding of the complex thinking about health and body weight. Our goal here is not to tell you how to think, eat, or live — nor is to to pass judgment on how you choose to nourish your body — but rather to start a conversation about diet culture, its impact, and how we might challenge the messages we are given about what makes us attractive, successful and healthy.
In February 2013, winter storm Nemo settled over Boston and it was A Bad One, even by New England standards. The roads were closed, taxi service shut down in a pre-Uber world and even the (semi) reliable T lurched to a stop for a day or two. We were all frozen in place in the final semester of my senior year of college. As city-wide cancellations poured in, undergrads stumbled out into the blustery and empty streets, heading toward our standby strip of bars, lobbing snowballs and sledding down Mission Hill as 85 MPH winds whipped the whiteness around. It was a joyous, beer-soaked snow globe — one I trudged right past on my way to the gym.
The next day, I was praised by hungover friends and snowed-in family members alike. “I wish I had your willpower!” “Ugh you’re so good!” and other commonplace, near-reflexive tropes we repeat when a person does something that seems healthy or shows superior discipline. This sustained behavior of mine — skipping out on social events for healthier choices like sticking to my exercise schedule, making measured and calorically scarce meals at home instead of dining out with friends, opting out of drinking to save the “empty” calories, tracking the nutritional content of my food — continued to net a thin body and likewise, a slew of compliments.
This sustained “healthy” behavior, in part, is also what landed me in treatment some 15 months later, diagnosed with a tangle of eating disorders, including one called orthorexia, which is an unhealthy focus on eating “healthily.” What may have started as me trying to eat for wellness had become obsessive and threatening to my actual health: Controlling my food and my weight had become my main priority, despite the fact that it was a detriment to my emotional and physical health. I withdrew from loved ones to avoid eating in public and developed a bad temper and poor attention span from sustained hunger. It also harmed my body — I lost my period, was extremely lethargic, had cholesterol issues and other problems college seniors aren’t supposed to face.
The diagnoses hit like a nor’easter — not only for me, but for nearly everyone in my periphery who’d lionized my dedication to being “fit and healthy.” It was so baffling! Even my doctors had praised me in the midst of my eating disorder, including an OB-GYN who, some months after my period stopped, eyeballed both me and my chart a couple times before saying, “I know you probably worked really hard to lose weight so I won’t ask you to put it back on.” And hadn’t I merely been living and eating the way our saved posts and Pins and favorite magazines suggested was ideal? Weren’t we supposed to celebrate fitness, healthy choices and the weight loss that (we hoped) came with them? Didn’t the “after” photos in all those ads and TV shows make it clear that thinness is the marker of success that comes with a healthy lifestyle change? How did this all make me sick — at risk of death, even?
Eating disorders have the second highest mortality rate of any mental illness. Although I — and others — had normalized and even admired my symptoms, the way I lived was life-threatening. And what made these formal diagnoses so scary and confusing, in part, is that they called into question a foundational yet hazardous pillar in our society: Diet and wellness culture, which wrongly conflate health with weight, and equate behaviors that lead to thinness (even when they are disordered) to “taking care of ourselves.” For me, labeling what I thought was good for me as “orthorexia” created ripples of introspection — and a whole lot of relearning — on what’s actually healthy behavior.
So what is orthorexia, exactly?
“Orthorexia nervosa is a condition characterized by exaggerated, obsessive, pathological fixation on healthy food, eating healthy or rather health-conscious eating,” says Rebecca Rialon Berry, Ph.D., Clinical Associate Professor at NYU Langone Health, characterized by an “obsession with clean eating, healthy eating [or] pure eating that is becoming more and more prevalent,” says Claire Mysko, CEO of National Eating Disorders Association (NEDA). While orthorexia isn’t an official diagnosis in the Diagnostic and Statistical Manual of Mental Disorders (DSM), the term is used “broadly in the field to describe that obsession with health, which can be, in many cases, masking disordered eating,” Mysko says.
Like better-known eating disorders, “Orthorexia is known to contribute to a number of negative mental health and medical complications, including malnutrition and nutritional deficits,” says Berry. And like the others, it can lead to life-threatening consequences “including anemia, osteoporosis, hormone imbalances and an abnormally slow heart-rate.” Veronica E. Garnett, M.S., R.D., C.C., Health at Every Size (HAES) registered dietitian and certified culinarian, concurs. Orthorexia, she says, has “a very real impact on [sufferers’] emotional, mental and physical health.”
What’s more, says Garnett, orthorexia is particularly sticky, since “there is no one perfect definition of health and there is no perfect definition of what makes a food healthy or not.” There are so many aspects of eating “healthy” a sufferer might fixate on: Is it the nutrients in the food? Is it the way it is produced? Is it certain ingredients believed to be healthful or the absence of others thought to be harmful? There are so many rabbit holes to hop down that the quest for “health” can be paralyzing. An example: An avocado, “according to the keto diet, [is] a ‘good’ food, but for a low-fat diet, it’s a ‘bad’ food,” says Garnett. “A person with orthorexia might see it as a ‘good’ food from a nutrition standpoint, but if it is not organic or locally produced it might be seen as a ‘bad’ food.” It is also not considered a low calorie food, which a sufferer might label “bad.” All this ambiguity can leave a vulnerable person constantly questioning her decisions, eating a rigidly narrow set of “approved” foods, or abstaining from eating altogether.
Of course, just as going to the gym instead of hanging out with friends on any given day is not inherently problematic, neither is researching an avocado’s nutritional value. Nor is adopting any number of theoretically healthful habits, such as introducing more vegetables to your diet, cooking more at home, looking at a menu before you head to a restaurant and so on. But when these “health” choices begin to dictate your life and become tied to your self worth — like, say, you’re skipping out on plans with friends to compulsively exercise in order to ward off feelings of perceived failure or lack of discipline — that’s where it can become a serious issue.
What causes orthorexia?
The specific causes of orthorexia are not established, says Berry, though people with certain personality characteristics seem to be more prone. “Obsessive-compulsive tendencies and prior or current eating disorders are known risk factors,” says Berry. “Other risk factors include tendencies toward perfectionism, high anxiety or a need for control.” Garnett agrees, saying “a history of dieting, a history of trauma, anxiety and depression, a perfectionist or controlling personality, substance abuse, etc.,” can also be contributing factors.
But while some people are more vulnerable than others to orthorexia, make no mistake: It’s a societal disease. “The biggest causes of orthorexia [are] diet and wellness culture, which are both rooted in white supremacy, anti-Blackness, and anti-fatness,” says Garnett. Berry agrees, adding that the “increasing cultural focus on health and wellbeing may contribute to orthorexia’s prevalence.” This coded “wellness diet,” says Christy Harrison, M.P.H., R.D., C.D.N., author of Anti-Diet and host of the Food Psych podcast, is a “sneaky modern guise of diet culture.”
It’s true that while “wellness” plans might not overtly mention weight, “the images of people who are held up as the picture of so-called wellness, they’re always thin,” says Harrison. In 2018, Weight Watchers rebranded to WW, “Wellness That Works,” yet at the time of publication of this article, the website’s homepage most prominently touts weight loss as its marker of success.
“People will say, ‘it’s not a diet, it’s a lifestyle change. It’s first about my health. It’s part of my wellness plan,’” says therapist Judith Matz, L.C.S.W., author of The Body Positivity Card Deck and Diet Survivor’s Handbook. “These are code words. Anytime a person manipulates their food for the purpose of weight loss, it is a diet and it is subject to the same pitfalls.”
How is orthorexia different from anorexia?
They can have quite a few things in common (and I am proof that you can have both at the same time), but “it can be difficult to distinguish between orthorexia and anorexia due to similarity in signs and symptoms, including intrusive, food-related thoughts, an increased amount of time spent thinking about food, strict behavior and rituals related to the preparation of meals, refusing to go out to eat, among others,” says Berry.
But there’s a key distinction between the two: Anorexia revolves around restriction for the purposes of weight loss, and orthorexia is centered around avoidance of foods the person feels are unhealthy. “Anorexia is defined by a difficulty maintaining body weight … the focus is on how food impacts body appearance and image representation,” says Berry. “Restriction per se is not the intention of the individual with orthorexia.” Rather, it’s about the person controlling what they eat in an attempt to consume only foods they deem healthy. Orthorexia also may look different than an eating disorder like bulimia or anorexia since the sufferer may not appear to be obsessed with weight control, thinness or body image. They may or may not be noticeably underweight.
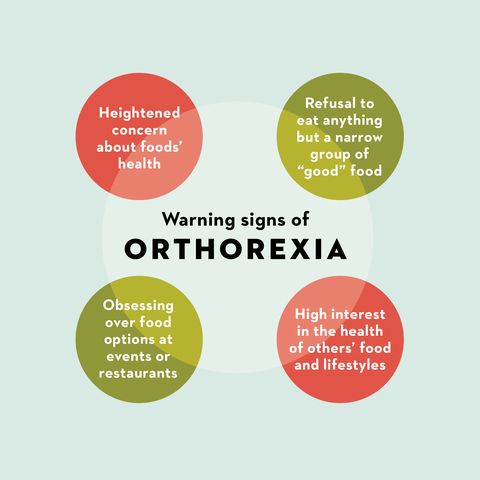
What are some warning signs and symptoms of orthorexia?
“For people with orthorexia, the pursuit of a ‘perfect’ diet takes up a significant amount of time and energy, and interferes with work, school and relationships,” says Berry. “A big warning sign of orthorexia is feeling unhinged or emotionally distressed around food,” says Garnett, which can “lead to negative changes in mood, guilt and shame around food choices, strained relationships,” as well as self-loathing and isolation.
But like many eating disorders and mental illnesses, orthorexia is often invisible, even to the person suffering. “People aren’t always aware of their eating disorders,” says Mysko. “One of the major tells that someone is not eating enough is that they think about food all day long,” adds Harrison (and for orthorexia, that’s with or without the conscious thought of wanting to be thinner). Other red flags include “obsessing about food and your weight, [or if] you find yourself weighing yourself frequently, or getting distracted by thoughts of food,” says Harrison. Here are some additional warning signs that your “wellness” plan is leading you down an unhealthy path, per NEDA:
- You compulsively check ingredients and nutritional labels, and have a heightened concern about ingredients’ health
- You cut out entire food categories (sugar, carbs, dairy, meat, etc.)
- You refuse to eat anything outside a narrow group of “healthy” or “clean”’ foods
- You take an unusual interest in the health of others’ food
- You obsess over what food may be available at events or restaurant, and are distressed when “clean” or “healthy” foods aren’t available
- You obsessively follow food and “healthy” lifestyle blogs on social media
- You’ve got body image concerns
Getting treatment for orthorexia
Orthorexia can be treated in similar ways to other eating disorders, with nutrition therapy and treatment models like Health at Every Size (HAES) and intuitive eating. “Cognitive-behavioral therapy for eating disorders (CBT-E) can be used to help an individual identify and replace distorted or harmful thoughts and beliefs about food,” says Berry, who adds that treatment may involve re-establishing a healthy weight and eating patterns to challenge food anxiety to develop tolerance and flexibility.
It’s hard to ask for help you don’t know you need, of course, but being your own advocate is so important when it comes to seeking treatment for suspected disordered eating or eating disorders. For me, I believed my quest for weight loss and all the behaviors that entailed was good for my health, until one night a switch flipped and I realized I might be treading in dangerous waters. I’d reached my goal weight and still wasn’t satisfied with my body. In fact, I was more self-conscious than ever! I couldn’t stop logging my calories and regularly overexercising into a deficit, my obsession with control ironically spinning out of control. When I came across the symptoms of anorexia while doing research for an article I was writing, my blood turned to ice in my veins. I knew. And I knew I wasn’t equipped to fix it alone.
Still, I kept this discovery to myself at first, living in the shadows of my own secret, and refusing to name it out loud. When I finally did call my doctor and a myriad of local therapists to ask for help, I was repeatedly turned away. All the therapists in my area had months-long waitlists, and my doctor’s office also said they couldn’t fit me in and suggested I call a crisis helpline… before immediately recanting and saying, “actually, those are reserved for life-threatening emergencies,” leaving me directionless and scared. I wish I’d known then that that the NEDA helpline is available to anyone on a daily basis, via call or text. Instead, I was suddenly terrified I might actually die before I could get the help I knew in my gut I needed.
But my experience is not uncommon, says Garnett. “It is very likely that [many] medical professionals do not have the experience or screening and diagnostic tools to adequately assess, diagnose, and refer patients for proper treatment,” says Garnett. A 2015 study found that medical training for eating disorders is limited, and there’s a need to “improve eating disorder diagnostic and treatment skills among trainees” across internal medicine, pediatrics, family medicine, psychiatry, and child and adolescent psychiatry. This is why of the 30 million Americans who experience a clinically significant eating disorder during their lifetime, only about one third of people ever receive treatment, according to the Alliance for Eating Disorder Awareness.
It was only once my dejection about the medical system had metamorphosed into rage — for myself and the other people who had been failed — that I was able to find help. I Googled “eating disorder recovery near me” and called the closest program to book an evaluation. The next week, I was seen in-office, and days later, admitted into partial hospitalization for treatment.
I was furious and relieved and terrified and… hopeful. That call was the best and the most important one I have ever made in my life, and I am so thankful someone answered it with the care I needed. Many others are not so lucky, or may not have the knowledge or self-awareness to know who to call. But even with the support, it still felt like jumping off a cliff in the dark with no safety net. I was finally looking the monster directly in the eyes, and I wasn’t even sure if I was ready to fight it — but I knew that I could never look away again.
Today, the monster is still there and I’ve learned it will always lurk. But it’s so much smaller and meeker than it once was, thanks to a toolkit I picked up in treatment and finessed in sustained therapy. Each time I win a stare-down is a victory, because recovery is an active, constant practice (this is why we say recovering not recovered).
These days I talk about EDs and my own struggles, past and present, openly with my loved ones — and, apparently now, in national publications — because darkness can’t thrive when light is shined. Sharing my experiences and admitting that I’m struggling leaves less room for the secrecy in which eating disorders thrive. “The healing journey does not have to be and should not be done alone or only on a 1:1 basis,” says Garnett. “Humans are pack animals. We need our tribe. We need community.” Here are some of her (and my) favorite resources, both online and in person:
Anyone feeling like they are suffering from disordered eating or an eating disorder can and should reach out for help immediately. The NEDA helpline at (800) 931-2237 is available daily via call or text, and officials also are on standby in digital chats, ready to help you find resources in your area. If you are concerned about a loved one, learn more about how you can help.
This content is created and maintained by a third party, and imported onto this page to help users provide their email addresses. You may be able to find more information about this and similar content at piano.io
Source link