One Man Is Sounding The Alarm After Yardwork Almost Killed Him

[ad_1]
While scrolling through social media last June, a shocking post caught my eye. A woman in my neighborhood described a mysterious ordeal involving her husband. Out of nowhere, the previously healthy man had gotten suddenly and severely ill. He had nearly died and was still fighting to recover. Like amateur sleuths, the family had been searching for the cause of his rapid decline. What they discovered, before even the doctors realized it, was terrifying, because it was something that could have just as easily happened to me, literally in my own backyard.
The first weekend of May last year, Jim LeBlond was busy with a familiar springtime ritual: clearing out his backyard. He was in a hurry because his city of Madeira, OH — a suburb of Cincinnati — offered curbside brush and limb pickup during the first week of May. “I worked an entire weekend clearing honeysuckle and the weeds around it with an electric chain saw,” Jim says. It had been a wet spring, and the weeds were already everywhere. “I saw a lot of white flowers, but I didn’t think anything of it.”
By the time Jim was taking the last batch of limbs out to the curb Monday evening, he started to feel bad. He wasn’t sure whether he was simply exhausted from a long weekend of work or he was coming down with something. COVID-19 briefly crossed his mind, but he was fully vaccinated. He decided to go to bed early, figuring he would probably feel better the next day.
Instead, at 4:00 a.m. Tuesday morning, he woke up unable to breathe. Frightened, he told his wife, Jeanne, that he needed to go to the emergency room, so they drove to nearby Good Samaritan Hospital. There, the emergency room doctor ran several tests but struggled to understand what was going on. Jim looked healthy, yet he clearly needed more and more oxygen. His chest X-ray showed inflammation. The ER doctor thought it was pneumonia and decided to admit him, still not having ruled out the coronavirus.
“I remember getting moved to a room,” Jim says. “But my memory of the next three weeks is totally blank.” That’s because things quickly deteriorated once Jim was admitted. He couldn’t breathe, and his oxygen levels were going down. He was being given COVID medications, but he kept testing negative. Within hours of being admitted, Jim was moved to the hospital’s intensive care unit (ICU). By 10:00 p.m. Wednesday evening, he had to be put on a mechanical ventilator. Jeanne wasn’t allowed into the ICU until 9:00 the following morning. “I walked into the room and immediately started to cry,” she says. Her 58-year-old husband had tubes down his throat and was sedated, in a medically induced coma. It seemed unfathomable given that only days earlier he had been laughing at dinner and playing on the floor with his grandchildren. What in the world had made him so sick?
Christopher Hayner, M.D., the pulmonary critical care physician at Good Samaritan Hospital who began treating Jim in the ICU, suspected an alveolar hemorrhage, which happens when “the blood vessels that surround the air sacs in the lungs become inflamed,” Dr. Hayner explains. This means the lungs can’t do their job of moving oxygen into the bloodstream as blood accumulates in the air sacs. “Essentially you drown in your own blood,” he says.
A biopsy confirmed the grim diagnosis. Now Dr. Hayner knew what was wrong, but no one knew why. Jim didn’t have any of the conditions, like lupus or other autoimmune diseases, that usually cause alveolar hemorrhage. Dr. Hayner ran test after test looking for what might be causing the extreme inflammation in Jim’s lungs — with no luck.
Unearthing the Shocking Cause
Once Dr. Hayner had ruled out all the common causes of alveolar hemorrhage, it was time to think about uncommon causes. He wondered whether Jim could have experienced some form of toxic inhalation injury, but there hadn’t been a fire or any use of toxic chemicals.
Jeanne is a retired elementary school teacher — for more than three decades, she had taught her young charges to be curious learners. Now she needed to use her own curiosity to solve the ghastliest puzzle she had ever encountered. She began to suspect that the problem was something Jim had cut down in the backyard. But he was unconscious, unable to offer any clues.
Jeanne and Jim both come from close-knit families, and their community in Madeira also rallied to help them. Their grown children, Jay and Kate, and their spouses, friends and family helped with tasks and alternated going with Jeanne to the ICU every day. They played Jim and Jeanne’s favorite song, “When You Say Nothing at All,” sung by Alison Krauss, which he and Jeanne had danced to at their 25th wedding anniversary 10 years earlier. They held his hand and talked to him, hoping he could hear them. “I was told many times he might not survive,” Jeanne says.
But Jim fought, and one morning when Jeanne arrived, the nurse said, “We have a surprise for you.” Jim was sitting in a chair for the first time in a month. “That was a big deal,” Jeanne says. “Finally, things looked like they were getting better.” He improved enough to be moved from the ICU to a step-down unit. He’d had a tracheostomy, so he still couldn’t talk, and he was still on a ventilator. He was extremely weak, unable even to push a button on the television remote to change the channel. “Lying there, you think you should be able to just get up and go home, but you can’t,” Jim says. He had a feeding tube because he couldn’t swallow or eat, and he had lost 42 pounds. Blood clots formed in his legs — common when someone is confined to a hospital bed — and he needed an IVC filter implanted in a blood vessel near his heart. This small device prevented the blood clots from traveling to his lungs and causing a fatal pulmonary embolism.
But he had gotten strong enough to write. At last he could be asked, “What were you cutting down in the backyard?”
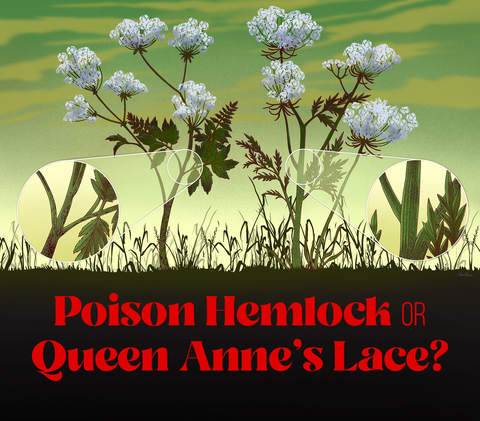
He wrote, White flower, purple stem. Though Jim was used to white flowers growing in his backyard, the ones he was familiar with were snakeroot, which doesn’t bloom until late in the summer. This time Jim had been working in his yard in early May, so it must have been something else. The family Googled “poisonous plants in Ohio,” and within seconds they had the prime suspect: a plant so toxic that it had been used as a poison for centuries — poison hemlock.
Swiping through the Web, they saw abundant images of poison hemlock in fields, on the sides of roads and at the edges of parks and playgrounds, and they read about how it had been invading specific states such as Ohio. It was tall and wispy, almost like giant parsley. It had blotchy purple stems and clusters of big white flowers. Had this been in their backyard?
They showed Jim the pictures. He nodded and wrote, That’s it.
According to Joe Boggs, an assistant professor of entomology for The Ohio State University Extension, poison hemlock contains highly toxic compounds and could cause respiratory failure and death if ingested. “The chemicals are in the sap, but the sap circulates throughout the whole plant, including the roots and seeds, so all parts of the plant are toxic,” Boggs says. The theory was that by taking a chain saw to it, Jim had aerosolized it, or thrown that sap into the air in the form of extremely fine droplets, which he then must have inhaled.
“I have to give the family credit for doing the deep dive and figuring out poison hemlock,” Dr. Hayner says. When he learned about the plant, he understood how it could have happened. “Anything you can touch, you can also inhale,” he says. The toxic aerosolized poison hemlock particles caused respiratory failure.
Jim’s case raised an alarm bell for Dr. Hayner, who had a large wooded hillside on his own property. He feared that poison hemlock might be lurking there as well. “We had been trying to clear the hill. The minute we figured this out, we stopped,” he says.
A Town Rallies and Raises Awareness
Dr. Hayner wasn’t the only one who was suddenly looking at every patch of weeds around, wondering if it possessed enough toxins to kill. I’d stop in the middle of runs and glower at wispy weeds on the side of the road, wondering if they were poison hemlock but afraid to get too close. It was as if my entire city of 9,000 was on the lookout. We read Jeanne’s Facebook updates about Jim, looked for purple stems and learned to tell the difference between poison hemlock and Queen Anne’s lace. Even then-mayor Nancy Spencer advocated educating the public about poison hemlock at a city council meeting. She included information about how to recognize it in a citywide newsletter and was looking for more ways to raise awareness about the invasive weed. Neighbors, friends and fellow church members rallied around the LeBlond family and provided continuous meal delivery through Jim’s hospital stay and beyond. They cut the family’s grass, re-stained their deck, made the house accessible and helped with medical bills. “People who didn’t even know us stepped up to help,” Jim says.
Ultimately Jim needed surgery on his heart, which had been damaged because of the problems with his lungs. He began to improve dramatically after the surgery and was finally able to come off the ventilator and the feeding tube in late July. As he began rehab at a facility in early August, he knew it would be a long road to recovery; sometimes five different physical therapists would work with him at once. With his tracheostomy removed, he had to relearn to talk and to swallow. It took an incredible amount of work for him to sit up on his own, stand and eventually walk. But this wasn’t the first time he’d had to relearn basic tasks. He had broken his hip in an accident when he was 14 and had then been in a wheelchair for nearly eight months. “I learned that you never tell a physical therapist no,” he says.
After 109 days, Jim finally came home on August 21. “There were many, many tears of joy that day,” Jeanne says. Everyone gathered for a welcome-home party, and the high school band played in the neighbors’ yard as Jim got out of the car. It would be several weeks before he could walk more than a few steps and several more weeks until he could play with his grandkids or drive again. He continues to do daily physical therapy to regain his strength, but the desire to do things like walk the dog and kick a soccer ball with his granddaughters again keeps him motivated. His recovery has already been miraculous, and his doctors anticipate that it will continue.
“Sometimes I think, What if our grandkids had picked those flowers?” Jeanne says. That’s why she and Jim want to do everything they can to help raise awareness about poison hemlock. Their community gave them so much, and they’re eager to pay it forward by helping make sure others’ backyards are safe.
Beware Poison Hemlock’s toxic cousin: Wild Parsnip
Poison hemlock is highly invasive and is in nearly every state in the U.S. It has especially become a problem in the Midwest and the South, says Joe Boggs, an assistant professor of entomology for The Ohio State University Extension. Wild parsnip, a slightly shorter plant with a flat cluster of yellow flowers, causes terrible blistering if the sap gets on skin and is exposed to sunlight. Here’s what to know about these two wild menaces, which often grow together:
- Where they grow: You are more likely to find these plants growing at the
edges of your property than you are to spot them amid your flower beds. - Why they are taking over: Land overdevelopment and overgrazing are big culprits. Mowing equipment that isn’t cleaned after the clearing of patches of these plants is also spreading the seeds.
- When you’ll see them: In spring and early summer. Both are generally done blooming by July.
- How to get rid of them: Never use a weed eater or a chain saw. If you wear protective clothing (goggles, gloves, mask, long sleeves and pants), you can pull up poison hemlock and bag it like other yard waste, Boggs says, but to be safe, you might consider using an herbicide to kill it. As for wild parsnip, do not touch it: Spray it with an herbicide.
- How to prevent their return: Once the poison hemlock or wild parsnip is dead, spread some grass seed as soon as you can. “Grasses are very strong competitors against these plants,” Boggs says.
[ad_2]
Source link